There are parallels between the denial on climate change and the need for a sustainable health service. The problem is that politicians are never willing to stick to an “unpalatable truth”, and the media are always willing to find a strap line that undermines any controversial aspect of change. The world is not celestial. We need compromising honesty in dealing with the reality and hard truths of this world. Health is little different from Social Care… Calls for increases in higher rate taxation usually result in more perverse activity above present levels, so it would have to be a tax on everyone. Co-payments for health would be a form of “deserts related” rationing, but the issue has to be faced. Nicola Bartlett reports in the Mirror that Norman Lamb suggests a “Tax on over 50s”. – and predictably John McDonnell slams Tories’ proposal to bring in a tax on ageing in order to fill a £2.75billion funding gap
Greg Hurst in the Times reports 29th April 2019: Call to fund elderly care with new tax
Tax rises should be introduced to fund a system that provides a standard level of social care for all elderly people in England in the same way as the basic state pension, a senior Conservative has said.
The Tory MP and former minister Damian Green added that older people should be encouraged to top up their care by paying for additional elements.
In a report for the Centre for Policy Studies think tank, Mr Green calculated that introducing a free entitlement to basic care at home or in a residential home would cost about £2.5 billion extra a year.
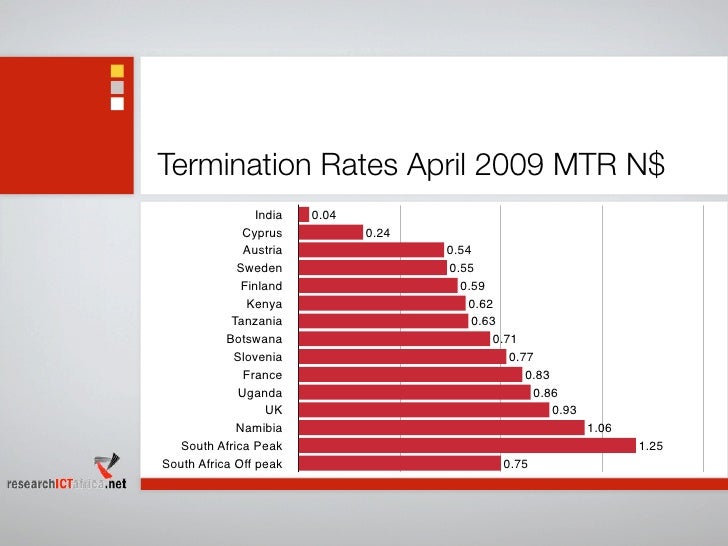
To pay for this he suggested that the winter fuel allowance, a tax-free payment of between £100 and £300, be withdrawn from pensioners who pay higher rate income tax. This would raise about £350 million a year. The rest could be funded with extra money from the Treasury’s spending review or, in the longer term, by imposing an additional national insurance rate of 1 per cent on the over-50s. This would mean that older taxpayers paid an extra £308 a year and would raise £2.4 billion.
The report suggested that a standard entitlement to universal social care would include a set number of hours of care at home per week or a bed in a care home with a minimum level of service, with people able to make top-up payments for extra services.
The Financial Times: Why UK is struggling to fix a mounting social care crisis
…A consultative social care “green paper” has missed a series of purported deadlines. Once promised “by April” officials now say only that it will appear “at the earliest opportunity”. …
…The King’s Fund, a leading health think-tank, last year projected that demand for social care would rise by about £12bn by 2030/31, growing at an average 3.7 per cent a year. With expenditure growing at just 2.1 per cent a year, the shortfall will be £1.5bn in 2020/21 and £6bn by 2030/31, at current prices. According to those familiar with the process of drafting the green paper, however, it will not propose a single definitive solution. The government’s caution is rooted in experience. The Conservative manifesto for the 2017 election said that people would have to pay all of their care costs until they were left with just £100,000 of assets. After an outcry, and warnings from her own backbenchers about a voter backlash, Mrs May said she would impose a cap on the total cost of social care bills facing middle class households. It is unclear whether a ceiling will be included in the green paper.